Dec . 04, 2024 10:04 Back to list
buy diagnosis of syphilis
Understanding the Importance of Diagnosing Syphilis A Comprehensive Overview
Syphilis, a sexually transmitted infection (STI) caused by the bacterium *Treponema pallidum*, has re-emerged as a significant public health concern in many parts of the world. Effective diagnosis and timely treatment are crucial in controlling its spread and preventing severe health complications. This article explores the various methods for diagnosing syphilis, the importance of early detection, and the implications for public health.
The Stages of Syphilis
Syphilis is characterized by several stages primary, secondary, latent, and tertiary. Each stage exhibits distinct clinical manifestations, making it essential for healthcare providers to recognize symptoms and risks associated with syphilis.
1. Primary Syphilis usually presents as a painless sore, known as a chancre, at the site of infection. This sore typically appears about three weeks after exposure. 2. Secondary Syphilis may develop weeks to months later, displaying symptoms like skin rashes, fever, sore throat, and swollen lymph nodes.
3. Latent Syphilis occurs when the infection is present but asymptomatic. Without treatment, this stage can persist for years.
4. Tertiary Syphilis can lead to severe complications affecting the heart, brain, and other organs and may occur years after the initial infection if untreated.
Diagnosis of Syphilis
The diagnosis of syphilis involves a combination of clinical evaluation and laboratory testing. There are several methodologies employed
1. Serological Tests
Serological testing is the most common diagnostic approach. These tests detect antibodies produced in response to the *Treponema pallidum* infection. They are typically categorized as
buy diagnosis of syphilis
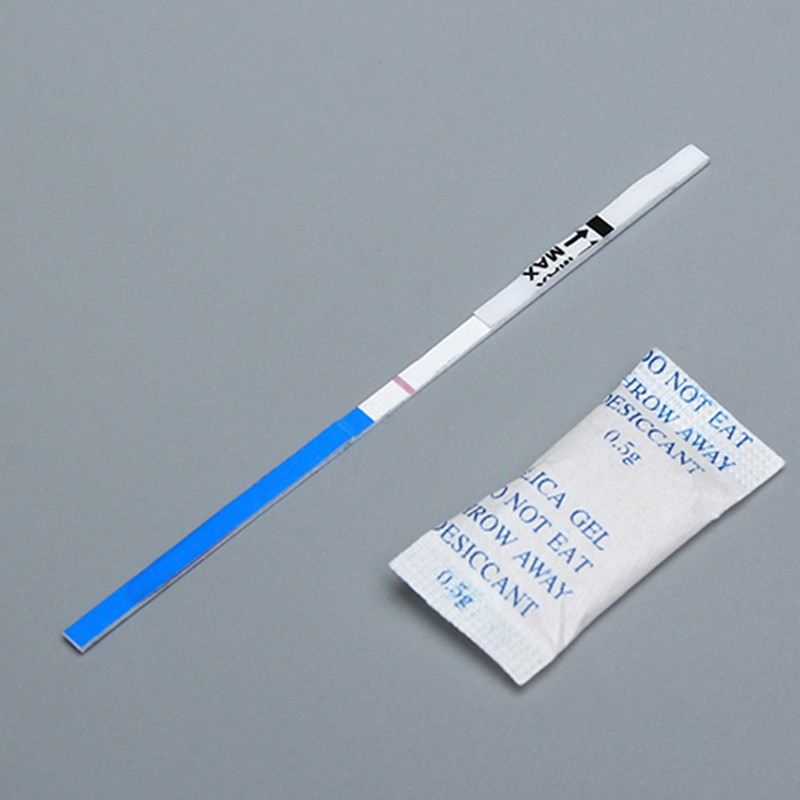
- Non-treponemal tests These include tests like the Rapid Plasma Reagin (RPR) and the Venereal Disease Research Laboratory (VDRL) tests. They are relatively easy to perform and are often used for screening. However, they can yield false positives due to various conditions like pregnancy or autoimmune diseases. - Treponemal tests These are more specific and include assays like the Treponema pallidum hemagglutination assay (TPHA) and the fluorescent treponemal antibody absorption test (FTA-ABS). These tests confirm the presence of *Treponema pallidum* antibodies and are typically used following a reactive non-treponemal test.
2. Clinical Evaluation
Healthcare professionals also rely on a detailed sexual history and physical examination. The identification of characteristic sores and rashes can guide physicians toward a syphilis diagnosis, especially in cases where lab tests are inconclusive.
3. Additional Testing
In some instances, healthcare providers may recommend further laboratory testing, such as a cerebrospinal fluid analysis, particularly in cases suspected of neurological involvement or if tertiary syphilis is a concern.
Importance of Early Detection
Early detection of syphilis is vital for several reasons
- Preventing Transmission Identifying and treating syphilis early can significantly reduce the risk of transmitting the infection to others. - Mitigating Health Complications Untreated syphilis can lead to severe health issues, including organ damage and increased risk of HIV infection.
- Ensuring Public Health Safety By diagnosing and treating syphilis early, health authorities can control outbreaks and manage the spread of STIs more effectively.
Conclusion
The diagnosis of syphilis is a critical component of public health efforts aimed at controlling sexually transmitted infections. Through a combination of serological testing and clinical evaluation, healthcare providers can effectively identify and treat syphilis, safeguarding not only individual health but also the community at large. Increasing awareness about syphilis and encouraging regular screenings can help minimize its impact and curb its resurgence in populations at risk. Public health campaigns and increased accessibility to testing are essential in fostering a healthier society free from the burdens of STIs.
-
Reliable Early Pregnancy Test Kit Supplier - Multi Plastic Cassette Options
NewsJul.30,2025
-
Transferrin Rapid Test Cassette – Reliable Tumor Marker Detection
NewsJul.29,2025
-
Accurate Follicle Stimulating Hormone Test Kit | Rapid Reliable Results
NewsJul.29,2025
-
High Accuracy LH Ovulation Test Kit - Digital Results & Wholesale Options
NewsJul.29,2025
-
HbsAg Blood Rapid Test Kit for Fast & Accurate Hepatitis B Detection
NewsJul.28,2025
-
Sterile Urine Cup for Safe & Easy Collection | High-Quality Specimen Cups
NewsJul.28,2025

