Oct . 20, 2025 10:45 Back to list
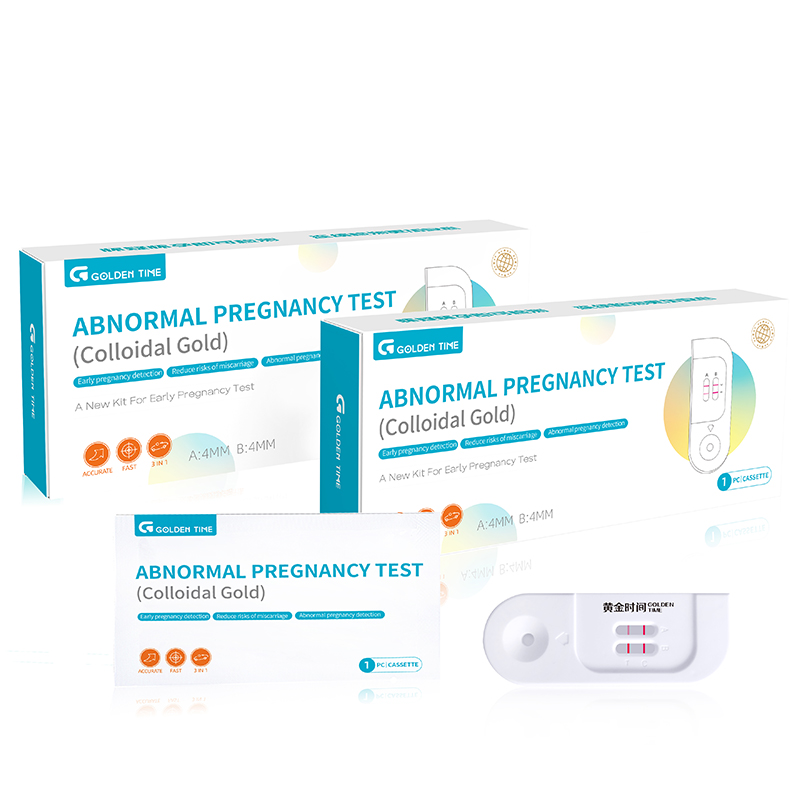
Abnormal Pregnancy Screening Test Kit – Fast, Accurate, Easy
What’s New (and Useful) in Early Risk Screening: A Journalist’s Take on Abnormal Pregnancy Testing
I’ve covered point-of-care diagnostics for a decade, and every year there’s a lateral-flow innovation that quietly changes practice. This season, it’s the abnormal pregnancy screening test kit from Goldentime—built to qualitatively detect intact hCG and hCGRP in urine and to flag risk for ectopic pregnancy or early loss. Sounds simple, but the implications at triage are big.
In plain terms: it’s a solid-phase, gold-labeled lateral flow immunoassay tuned not just to “pregnant or not,” but to the structure of hCG variants. In fact, that structural nuance is what clinicians have been asking for in early-risk assessment. Many customers say it reduces second-guessing when ultrasound access is delayed—which, to be honest, happens more often than we like in busy ERs and remote clinics.
How it’s built and why it matters
- Materials: nitrocellulose membrane, gold-conjugated anti-hCG/hCGRP antibodies, sample pad, absorbent pad, plastic cassette.
- Method: lateral flow immunochromatography with dual-epitope capture to differentiate intact hCG from related proteins.
- Intended use: qualitative detection for pregnancy confirmation plus risk assessment of abnormal pregnancy patterns.
- Service life: shelf life ≈ 24 months (unopened); use within 1 hour after pouch opening; store 2–30°C, no freezing.
- Industries: emergency departments, urgent care, OB/GYN clinics, community health, telemedicine kits, pharmacy screening corners.
Product specifications (field realities included)
| Analytes | Intact hCG + hCGRP (qualitative) |
| Sample type | Urine (first-morning preferred, but not mandatory) |
| LoD (hCG) | ≈ 20 mIU/mL (real-world use may vary with matrix) |
| Time to result | 5–10 minutes |
| Accuracy | Positive agreement ≈ 98–100% at ≥25 mIU/mL; negative agreement ≥99% (CLSI EP12-style evaluations) |
| Standards & QA | Manufacturing under ISO 13485; performance verification aligned to CLSI EP12-A2/EP17; stability per ISO 23640 |
Process flow (from carton to call)
- Receive kits (origin: No.136, Shiji West Road, Gaobeidian City, 074000, Hebei, China). Check lot, expiry, and storage log.
- Collect urine in a clean container; avoid preservatives. Let it reach room temp.
- Dip or drop: 3–4 drops into sample well. Start timer.
- Read at 5–10 minutes. Don’t interpret after 15 minutes.
- Document result in LIS or logbook. For suspected ectopic patterns, follow local protocols immediately (ultrasound, serial β‑hCG, etc.).
Where it’s used (and what users report)
ER triage, rural clinics, and mobile women’s health teams use the abnormal pregnancy screening test kit to flag risk while arranging imaging. Surprisingly robust in heat—though, yes, stick to the storage spec. Feedback has been that the additional structural signal reduces “false reassurance” in borderline early cases.
Vendor snapshot (because procurement cares)
| Vendor | Key Differentiator | Certs & Status | MOQ / Lead Time |
|---|---|---|---|
| Prises Bio (Goldentime) | Dual-target (hCG + hCGRP) risk signal | ISO 13485; CE-IVD applicability by market | Around 5k–10k pcs / 3–5 weeks |
| Brand X | Standard hCG only | ISO 13485; CE on select SKUs | 10k+ / 4–6 weeks |
| Brand Y | Cassette + midstream formats | ISO 13485; regional registrations vary | 5k+ / 4 weeks |
Customization options
- Private label, IFU localization (EN/ES/FR/AR, etc.).
- Cassette branding, barcode/UDI, pouch artwork.
- Bulk strips for OEM integration and combo panels.
Mini case study: rural triage
A county clinic piloted the abnormal pregnancy screening test kit in a nurse-led protocol. Over three months, time-to-ultrasound prioritization improved—patients with concerning qualitative patterns were fast-tracked the same day. Not a randomized trial, sure, but staff say it reduced overnight returns and “what-if” calls.
Note: This device supports clinical decision-making and does not replace imaging or serial quantitative β‑hCG per local guidelines.
References
- CLSI EP12-A2. User Protocol for Evaluation of Qualitative Test Performance, 2nd ed.
- ISO 23640:2011. IVD medical devices—Stability evaluation of IVD reagents.
- ACOG Practice Bulletin No. 193: Tubal Ectopic Pregnancy.
- WHO. Managing complications in pregnancy and childbirth: Ectopic pregnancy guidance.
-
Fast Syphilis Test: Rapid, Reliable Diagnostics for Global Health
NewsNov.20,2025
-
Serology Syphilis Test: Global Importance and Latest Diagnostic Advances
NewsNov.20,2025
-
Diagnose Syphilis Test – Essential Screening & Diagnostics Explained
NewsNov.19,2025
-
Comprehensive Guide to Diagnosis Syphilis Test Technologies & Applications
NewsNov.19,2025
-
Comprehensive Guide to Syphilis Test Dubai – Early Detection & Reliable Screening
NewsNov.18,2025
-
Comprehensive Guide to Syphilis Test Diagnosis: Global Impact and Advances
NewsNov.18,2025

